جراحی فک
What is a maxillary orthognathic surgery?
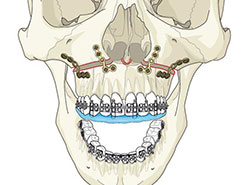
In simple terms orthognathic surgery means surgery of the jawbones. The surgery will be necessary to properly , align the maxilla or upper jaw and or the mandible or lower jaw to the other facial bones and the base of the skull. Proper alignment helps to insure the long-term success of the orthodontics, protects the teeth and tooth supporting structures, improves function of the jaws and also decreases the potential for overloading forces on the temporomandibular joints (jaw joint) and facial muscles.According to the nature of the problem, orthognathic surgery can be performed in the upper jaw or the lower jaw or both.Upper jaw surgery is accomplished through a small incision in the gum tissue above the teeth. Once a cut is made through the bone, the upper jaw and the bone that forms the roof of the mouth can be repositioned to fix the bite. It can be moved forwards or backwards. It can also be moved up or down depending on the aesthetic needs of the patient. The upper jaw is held in it’s new location using tiny titanium metal plates.
Am I a candidate for a maxillary orthognathic surgery?
The purpose of orthognathic surgery is to correct functional and esthetic problems that are due to underlying skeletal deformities. Severe malocclusion (bad bite) may cause many functional problems. You may have already experienced some of the following: inability to chew food properly which compromises digestion; speech problems; facial dysfunction characterized by headaches, joint pain, and periodontal trauma. Orthognathic surgery is also an important part of the treatment of obstructive sleep apnea.Orthognathic surgery if often the treatment solution in cases where the bite problem is so severe that orthodontic treatment alone isn’t enough to correct the problem, or where orthodontics alone would compromise your facial appearance.
Overjet
This term means the lower teeth are horizontally behind the upper teeth. The orthodontists refer to this as overjet. the normal overjet is about 2 mm, and in the case more than 2 mm it is classified as a Class II malocclusion. The cause might be an undergrowth of the lower jaw or the over growth of the upper jaw and is a reflection of the inherited genetic pattern. The growth problem is the reason of a malocclusion and this is reflected in the facial profile. The over growth of the upper jaw can be corrected by setting back the upper jaw by performing a maxillary setback orthognathic surgery.
Reverse Overjet
A reverse overjet is the opposite of Class II malocclusion with the upper teeth actually hitting behind the lower incisors and is referred to as a Class III malocclusion.The cause might be an over growth of the lower jaw or the under growth of the upper jaw and is a reflection of the inherited genetic pattern. The growth problem is the reason of a malocclusion and this is reflected in the facial profile. The under growth of the upper jaw can be corrected by advancing the upper jaw by performing a maxillary advancement orthognathic surgery.
Open Bite
Normally the upper incisors should cover the 2 mm superior portion of the lower incisors. In the case of the lack of the coverage, open bite occurs. Open bites are among the most difficult dentoskeletal patterns for orthodontists to treat. The surgery to correct an open bite in the adult involves a Maxillary Osteotomy, usually impaction of the back part of the upper jaw, allowing the lower jaw to rotate closed. In some cases both jaw orthognathic surgery is needed for the correction of the open bite problem.
Treatment of Long-face and Gummy Smile
Many gummy smiles can be a result of short teeth, a short upper lip, upright maxillary incisors, an excessive mobility to smile, and vertical overgrowth of the upper jaw. The vertical overgrowth of the upper jaw is often referred to as the “long face syndrome” and is characterized by a long lower facial third, an inability to get lips together at rest, and a gummy smile. The long face syndrome or vertical overgrowth of the top jaw is very often accompanied by an open bite malocclusion, and surgical correction of the bite is performed through the Lefort I Osteotomy where the upper jaw is moved upward to close the bite, which in turn diminishes the amount of gumminess of the smile.
Treatment of Short Face
Just as an upper jaw may grow too far vertically, in many cases, it may not grow vertically enough. This is in turn characterized as the “short face syndrome” and is characterized by a short lower facial third and incomplete incisor display on smile. In this case, lengthening of the face provides a better proportionality as well as improving the appearance of the lips.
How do I prepare for a maxillary orthognathic surgery?
THE INITIAL VISIT
At the first visit, a set of diagnostic records will be taken to determine the nature of your problem and what can be done to correct that problem. After processing and analyzing those records, we will meet with you for a consultation appointment to discuss your treatment options. The following explains the individual records that may be taken and what their purpose is:
Photographs
Frontal, oblique, and side facial photographs are part of the overall work-up of the case. These facial pictures serve as visual aids for bony and soft tissue analysis so that the facial aspects of treatment can be thoroughly evaluated. Photographs of the teeth will also be taken to provide an accurate record of the mouth at the time treatment begins.
Cephalopmetric (Lateral Skull) Radiograph
This side view radiograph of the face allows us to compare your tooth and jaw relationships to normal or ideal measurements.
Panoramic Radiograph
The panoramic radiograph is a composite radiograph of the teeth as well as both jaws. In one film, it shows us if you have the normal number of teeth, wisdom teeth, missing teeth, impacted teeth or extra teeth.
Study Models
Dental models will be used to study the dental problems as they exist at the beginning of treatment and are used for reference during pre-treatment planning.
CONSULTATION APPOINTMENT
While surgery may be the best option to achieve desirable functional and cosmetic results, it is always an elective procedure. Other treatment options will be presented to you in the consultation appointment. In this visit, we will discuss:
• The overall analysis and problem list
• Treatment objectives
• The anticipated treatment sequence
• Optional treatment plans and their strengths and weaknesses relative to your overall treatment objectives
Because treatment in adults often involves more complex problems, referrals to other specialists may be necessary. Also, if we find that tooth removal is required for orthodontic purposes, a referral will be made to your dentist or oral surgeon at that time.
How is a maxillary orthognathic surgery performed?
PRESURGERY
The following is a general sequence of events that occurs once your treatment begins. Please remember that each treatment plan and case may vary from this general sequence of events.
In order to prepare your teeth for your orthognathic procedure, we will place braces on your teeth to begin their alignment. The purpose of the presurgical phase of orthodontics is generally to:
• Align crowded teeth
• Decompensate incisors (align them properly within the jawbone)
• Coordinate the teeth so they will fit when the surgery is performed
Presurgical orthodontics may take as few as 6 months or as many as 18 months, depending on your needs. During your treatment, impressions will be taken in order to check the progress of the orthodontic alignment.
The Surgical Work-up
When the presurgical phase of orthodontics is complete, radiographs, photos and models will once again be gathered at this important appointment. Our final surgical plans will be determined from the work-up records.
THE SURGERY
Day of Surgery
Generally, you will be admitted to the hospital the morning of your scheduled surgery. The length of your surgery depends on the procedure being performed. The length of your hospital stay also varies according to your procedure.
POST SURGERY
Postoperative Orthodontic Treatment
Orthodontic treatment after surgery usually takes between 6-12 months.
Appliance Removal and Retainers
This is the day you have waited for-the day your braces are removed! Most often, a fixed retainer will be bonded to the inside of the lower front teeth before removing the braces. The upper retainer is usually removable. One week after removing your braces, you will receive this retainer and instructions on care and use.
Recall Visits
Further appointments with us are necessary after your braces have been removed. These periodic visits will be every 3-6 months and are necessary to adjust your retainer and check your bite.
Equilibration and Final Restorative Dentistry
In some cases, “equilibration” may be needed. Equilibration is simply the “fine-tuning” of your bite and is done by your dentist. Any bridges, replacement crowns, etc. should also be done at this time.
Are there different types of maxillary orthognathic procedures?
Maxillary orthognathic surgery is usually performed by LeFort I Osteotomy. This operation involves the upper jaw (maxilla) and the movement of it in various directions. According to the direction of the upper jaw movement there are several maxillary orthognathic procedures:
• Maxillary advancement surgery
• Maxillary set-back surgery
• Maxillary inferior repositioning
• Maxillary superior repositiong
What results can I expect?
During the healing period (6 weeks) you must have a modified diet. This generally means that one starts with fluids only, then graduates to a restricted diet and later to a non-chew diet. Our dietitian will be happy to help should you have special dietary requirements. Moderate swelling of the face can be expected and in some cases bruising occurs. This begins to subside 2-3 days after surgery. Expect to take 7-14 days off work in a sedentary occupation and a little longer if your job involves physical activity. After discharge from hospital, your surgeon will review your progress 1-2 weekly for the first six weeks. He may use rubber bands to ensure that your bite remains in the appropriate position. After this period you will return to your orthodontist.
What is involved in recovery?
We do everything we can to make your surgical experience as comfortable as possible. There are several things you can do to help.
Swelling
The amount of postoperative swelling which occurs varies from person to person. It appears to be greater in the second or third day after surgery and tends to decrease thereafter. Swelling may be present up to 6 months after your surgery, but generally is only noticeable up to 6 weeks. In order to minimize swelling, we suggest:
• Ice compresses – It is most important that ice compresses be in place the first 12 hours after surgery.
• Elevation of head – (The first 2 weeks after surgery) The head should be placed at a 30-45 degree angle while sleeping.
• Steroids – Your surgeon may recommend the administration of steroids to reduce the amount of swelling.
• Increasing activities – Walking and “getting back to normal” increases blood flow, which helps to disperse swelling. We encourage all patients to begin normal walking and other activities which would increase their blood flow.
Resuming Normal Activities
Most patients return to work or school one week after their procedure. Physical activities such as jogging, working out, etc., should not be resumed for approximately 3 months. Walking and other more moderate activities are certainly encouraged in order to increase your blood flow to reduce swelling, as well as to improve your frame of mind.
Oral Hygiene
Strict oral hygiene maintenance is essential. If you do not keep your mouth clean after your surgical procedure, you greatly increase the chance of an infection occurring. Use a soft bristle brush, preferably with a very small head (child’s toothbrush), and clean above the brackets and around the orthodontic archwires as effectively as possible.
Clear Fluids
As soon as possible after surgery, you will be encouraged to drink clear fluids. You will usually be able to drink directly from cup or glass and the use of a straw is rarely necessary. It is important that you drink adequately so the intravenous fluids may be discontinued. An average adult requires approximately 2.5 to 3 liters of fluid a day.
Is a maxillary orthognathic surgery safe?
• Pain – Some pain can be anticipated, but in most cases it is mild to moderate and satisfactorily controlled with analgesic medications. You should also expect to have a sore throat following your surgery. The soreness is caused by the irritation of the anaesthetic breathing tube and also the presence of a throat pack used during the procedure. The soreness of the throat rarely lasts longer then several days.
• Swelling – Swelling is a normal after-effect of surgery, the degree of which varies between individuals. More swelling usually occurs with lower jaw surgery than with surgery involving the upper jaw, and usually peaks the day after the operation. Your appearance will begin to improve as the swelling resolves. Swelling of the lips can be minimised by applying a medicated cream which will be prescribed in some cases.
• Bleeding – It is common to experience some minor bleeding following surgery, and minor nose bleeds may be expected for a period of one to two weeks following upper jaw surgery.
• Infection – Infection is possible after any type of surgery. You will be given antibiotics both during, as well as after the operation to help prevent this. If an infection should develop it is usually very easily treated.
• Tingling/Numbness – You will experience altered sensation or numbness, in the upper teeth following an upper jaw procedure. While the nerve fibres are healing, you may encounter strange sensations or tingling. Normal sensation usually returns in six months or less. On rare occasions, the altered sensation may be permanent.
• Nasal Congestion – Nasal congestion may occur both from the tube(s) placed in the nostrils during surgery and also from surgical procedures involving the upper jaw. When this occurs, the congestion can be managed by using nasal sprays and cleansing the nostrils. The nasal congestion will usually resolve 1 to 2 weeks after surgery.
• Weight Loss – Weight loss of 2-5 Kg may be anticipated during the early post-operative period. In most cases, this is due to a loss of appetite coupled with the wearing of elastics. After the first week, your appetite should have improved enough to maintain and possibly increase your weight.
• Post-Surgical Movement (Relapse) – When teeth and jaws are moved by orthodontics and surgery, the goal is to place them in a more favourable position. Many forces have been responsible for the growth and consequent positioning of the jaws and teeth. The muscular forces that caused the original growth problem and the jaw relationship are still present. As a result, there is a small chance that the jaw(s) and teeth will move back towards their original position. This is termed relapse. Many things are done throughout treatment to counteract relapse, but some degree of relapse almost always occurs.
Mandibular Surgery
What is a mandibular orthognathic surgery?
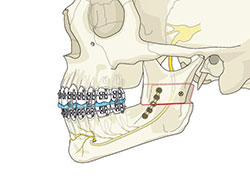
In simple terms orthognathic surgery means surgery of the jawbones. The surgery will be necessary to properly , align the maxilla or upper jaw and or the mandible or lower jaw to the other facial bones and the base of the skull. Proper alignment helps to insure the long-term success of the orthodontics, protects the teeth and tooth supporting structures, improves function of the jaws and also decreases the potential for overloading forces on the temporomandibular joints (jaw joint) and facial muscles.According to the nature of the problem, orthognathic surgery can be performed in the upper jaw or the lower jaw or both.Lower jaw surgery is accomplished by cutting the lower jaw in such a fashion as to allow it to slide on itself, much like a sliding glass door would slide open or closed. Through this technique the jaw can be advanced and lengthened or reduced and shortened.
Am I a candidate for a mandibular orthognathic surgery?
The purpose of orthognathic surgery is to correct functional and esthetic problems that are due to underlying skeletal deformities. Severe malocclusion (bad bite) may cause many functional problems. You may have already experienced some of the following: inability to chew food properly which compromises digestion; speech problems; facial dysfunction characterized by headaches, joint pain, and periodontal trauma. Orthognathic surgery is also an important part of the treatment of obstructive sleep apnea.Orthognathic surgery if often the treatment solution in cases where the bite problem is so severe that orthodontic treatment alone isn’t enough to correct the problem, or where orthodontics alone would compromise your facial appearance.
Overjet
This term means the lower teeth are horizontally behind the upper teeth. The orthodontists refer to this as overjet. the normal overjet is about 2 mm, and in the case more than 2 mm it is classified as a Class II malocclusion. The cause might be an undergrowth of the lower jaw or the over growth of the upper jaw and is a reflection of the inherited genetic pattern. The growth problem is the reason of a malocclusion and this is reflected in the facial profile. The under growth of the lower jaw can be corrected by advancing the lower jaw by performing a mandibular advancement orthognathic surgery. The lower jaw can be lengthened through a Bilateral Sagittal Split Osteotomy, which allows bony contact throughout the procedure and permits placement of direct rigid fixation-which means the teeth are not wired together and you can open your mouth after surgery.
Reverse Overjet
A reverse overjet is the opposite of Class II malocclusion with the upper teeth actually hitting behind the lower incisors and is referred to as a Class III malocclusion.The cause might be an over growth of the lower jaw or the under growth of the upper jaw and is a reflection of the inherited genetic pattern. The growth problem is the reason of a malocclusion and this is reflected in the facial profile. The over growth of the lower jaw can be corrected by setting back the lower jaw by performing a mandibular setback orthognathic surgery. The lower jaw can be shortened through the use of the Bilateral Sagittal Split Osteotomy, which allows bony contact throughout the procedure and permits placement of direct fixation.
Open Bite
Normally the upper incisors should cover the 2 mm superior portion of the lower incisors. In the case of the lack of the coverage, open bite occurs. Open bites are among the most difficult dentoskeletal patterns for orthodontists to treat. The surgery to correct an open bite in the adult involves a Maxillary Osteotomy, usually impaction of the back part of the upper jaw, allowing the lower jaw to rotate closed. In some cases both jaw orthognathic surgery is needed for the correction of the open bite problem.
How do I prepare for a mandibular orthognathic surgery?
THE INITIAL VISIT
At the first visit, a set of diagnostic records will be taken to determine the nature of your problem and what can be done to correct that problem. After processing and analyzing those records, we will meet with you for a consultation appointment to discuss your treatment options. The following explains the individual records that may be taken and what their purpose is:
Photographs
Frontal, oblique, and side facial photographs are part of the overall work-up of the case. These facial pictures serve as visual aids for bony and soft tissue analysis so that the facial aspects of treatment can be thoroughly evaluated. Photographs of the teeth will also be taken to provide an accurate record of the mouth at the time treatment begins.
Cephalopmetric (Lateral Skull) Radiograph
This side view radiograph of the face allows us to compare your tooth and jaw relationships to normal or ideal measurements.
Panoramic Radiograph
The panoramic radiograph is a composite radiograph of the teeth as well as both jaws. In one film, it shows us if you have the normal number of teeth, wisdom teeth, missing teeth, impacted teeth or extra teeth.
Study Models
Dental models will be used to study the dental problems as they exist at the beginning of treatment and are used for reference during pre-treatment planning.
CONSULTATION APPOINTMENT
While surgery may be the best option to achieve desirable functional and cosmetic results, it is always an elective procedure. Other treatment options will be presented to you in the consultation appointment. In this visit, we will discuss:
• The overall analysis and problem list
• Treatment objectives
• The anticipated treatment sequence
• Optional treatment plans and their strengths and weaknesses relative to your overall treatment objectives
Because treatment in adults often involves more complex problems, referrals to other specialists may be necessary. Also, if we find that tooth removal is required for orthodontic purposes, a referral will be made to your dentist or oral surgeon at that time.
How is a mandibular orthognathic surgery performed?
PRESURGERY
The following is a general sequence of events that occurs once your treatment begins. Please remember that each treatment plan and case may vary from this general sequence of events.
In order to prepare your teeth for your orthognathic procedure, we will place braces on your teeth to begin their alignment. The purpose of the presurgical phase of orthodontics is generally to:
• Align crowded teeth
• Decompensate incisors (align them properly within the jawbone)
• Coordinate the teeth so they will fit when the surgery is performed
Presurgical orthodontics may take as few as 6 months or as many as 18 months, depending on your needs. During your treatment, impressions will be taken in order to check the progress of the orthodontic alignment.
The Surgical Work-up
When the presurgical phase of orthodontics is complete, radiographs, photos and models will once again be gathered at this important appointment. Our final surgical plans will be determined from the work-up records.
THE SURGERY
Day of Surgery
Generally, you will be admitted to the hospital the morning of your scheduled surgery. The length of your surgery depends on the procedure being performed. The length of your hospital stay also varies according to your procedure.
POST SURGERY
Postoperative Orthodontic Treatment
Orthodontic treatment after surgery usually takes between 6-12 months.
Appliance Removal and Retainers
This is the day you have waited for-the day your braces are removed! Most often, a fixed retainer will be bonded to the inside of the lower front teeth before removing the braces. The upper retainer is usually removable. One week after removing your braces, you will receive this retainer and instructions on care and use.
Recall Visits
Further appointments with us are necessary after your braces have been removed. These periodic visits will be every 3-6 months and are necessary to adjust your retainer and check your bite.
Equilibration and Final Restorative Dentistry
In some cases, “equilibration” may be needed. Equilibration is simply the “fine-tuning” of your bite and is done by your dentist. Any bridges, replacement crowns, etc. should also be done at this time.
Are there different types of mandibular orthognathic procedures?
Mandibular orthognathic surgery is usually performed by Sagittal Split Osteotomy. This operation is performed on the lower jaw (mandible) in order to move it forward (in the case of a deficient lower jaw), or backward (in the case of a large lower jaw). It is performed behind the back teeth (not in the joint) and the jaw is sectioned in such a way that bony contact is always maintained. There are no gaps in the bone that have to be filled in, and it is not necessary to wire your teeth together during the postoperative healing period.
What results can I expect?
During the healing period (6 weeks) you must have a modified diet. This generally means that one starts with fluids only, then graduates to a restricted diet and later to a non-chew diet. Our dietitian will be happy to help should you have special dietary requirements. Moderate swelling of the face can be expected and in some cases bruising occurs. This begins to subside 2-3 days after surgery. Expect to take 7-14 days off work in a sedentary occupation and a little longer if your job involves physical activity. After discharge from hospital, your surgeon will review your progress 1-2 weekly for the first six weeks. He may use rubber bands to ensure that your bite remains in the appropriate position. After this period you will return to your orthodontist.
What is involved in recovery?
We do everything we can to make your surgical experience as comfortable as possible. There are several things you can do to help.
Swelling
The amount of postoperative swelling which occurs varies from person to person. It appears to be greater in the second or third day after surgery and tends to decrease thereafter. Swelling may be present up to 6 months after your surgery, but generally is only noticeable up to 6 weeks. In order to minimize swelling, we suggest:
• Ice compresses – It is most important that ice compresses be in place the first 12 hours after surgery.
• Elevation of head – (The first 2 weeks after surgery) The head should be placed at a 30-45 degree angle while sleeping.
• Steroids – Your surgeon may recommend the administration of steroids to reduce the amount of swelling.
• Increasing activities – Walking and “getting back to normal” increases blood flow, which helps to disperse swelling. We encourage all patients to begin normal walking and other activities which would increase their blood flow.
Resuming Normal Activities
Most patients return to work or school one week after their procedure. Physical activities such as jogging, working out, etc., should not be resumed for approximately 3 months. Walking and other more moderate activities are certainly encouraged in order to increase your blood flow to reduce swelling, as well as to improve your frame of mind.
Oral Hygiene
Strict oral hygiene maintenance is essential. If you do not keep your mouth clean after your surgical procedure, you greatly increase the chance of an infection occurring. Use a soft bristle brush, preferably with a very small head (child’s toothbrush), and clean above the brackets and around the orthodontic archwires as effectively as possible.
Clear Fluids
As soon as possible after surgery, you will be encouraged to drink clear fluids. You will usually be able to drink directly from cup or glass and the use of a straw is rarely necessary. It is important that you drink adequately so the intravenous fluids may be discontinued. An average adult requires approximately 2.5 to 3 liters of fluid a day.
Is a mandibular orthognathic surgery safe?
• Pain – Some pain can be anticipated, but in most cases it is mild to moderate and satisfactorily controlled with analgesic medications. You should also expect to have a sore throat following your surgery. The soreness is caused by the irritation of the anaesthetic breathing tube and also the presence of a throat pack used during the procedure. The soreness of the throat rarely lasts longer then several days.
• Swelling – Swelling is a normal after-effect of surgery, the degree of which varies between individuals. More swelling usually occurs with lower jaw surgery than with surgery involving the upper jaw, and usually peaks the day after the operation. Your appearance will begin to improve as the swelling resolves. Swelling of the lips can be minimised by applying a medicated cream which will be prescribed in some cases.
• Bleeding – It is common to experience some minor bleeding following surgery, and minor nose bleeds may be expected for a period of one to two weeks following upper jaw surgery.
• Infection – Infection is possible after any type of surgery. You will be given antibiotics both during, as well as after the operation to help prevent this. If an infection should develop it is usually very easily treated.
• Tingling/Numbness – You will experience altered sensation or numbness, in the upper teeth following an upper jaw procedure. While the nerve fibres are healing, you may encounter strange sensations or tingling. Normal sensation usually returns in six months or less. On rare occasions, the altered sensation may be permanent.
• Nasal Congestion – Nasal congestion may occur both from the tube(s) placed in the nostrils during surgery and also from surgical procedures involving the upper jaw. When this occurs, the congestion can be managed by using nasal sprays and cleansing the nostrils. The nasal congestion will usually resolve 1 to 2 weeks after surgery.
• Weight Loss – Weight loss of 2-5 Kg may be anticipated during the early post-operative period. In most cases, this is due to a loss of appetite coupled with the wearing of elastics. After the first week, your appetite should have improved enough to maintain and possibly increase your weight.
• Post-Surgical Movement (Relapse) – When teeth and jaws are moved by orthodontics and surgery, the goal is to place them in a more favourable position. Many forces have been responsible for the growth and consequent positioning of the jaws and teeth. The muscular forces that caused the original growth problem and the jaw relationship are still present. As a result, there is a small chance that the jaw(s) and teeth will move back towards their original position. This is termed relapse. Many things are done throughout treatment to counteract relapse, but some degree of relapse almost always occurs.
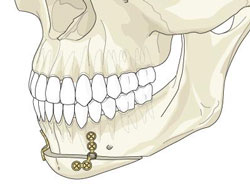
Chin Surgery (Genioplasty)
What is genioplasty (chin surgery)?
Chin surgery aims at reshaping the chin by enhancement with an implant, by cutting the boney chin and moving it forward (genioplasty), or by reduction of the chin bone. It’s not uncommon for chin surgery to be performed in addition to other facial surgery procedures to give the best overall facial balance.We have used chin surgery techniques to create symmetry among your facial features by establishing balance and proportion. Your procedure may be performed alone, or as a complement to other facial contouring procedures such as face lift, neck lift, cosmetic nose surgery (rhinoplasty) or other procedures.
Am I candidate for chin surgery?
Chin surgery is highly individualized procedures, with the best results achieved by a thorough consultation with your surgeon.
Good candidates for chin surgery include:
• Individuals whose facial bones have reached physical maturity, which generally occurs in late adolescence
• Individuals who are bothered by a small chin, weak jaw or lack of facial contour
• Healthy individuals who have no major medical conditions
How do I prepare for facial implant and chin surgery?
Preparing for your chin surgery procedures at our clinic may include:
• Lab testing or a medical evaluation
• Taking certain medications or adjusting your current medications
• Stopping smoking well in advance of surgery
• Avoiding aspirin, anti-inflammatory drugs and herbal supplements due to increased risk of bleeding.
How is chin surgery performed?
Genioplasty is a procedure that can be an alternative to the chin implant as no implant is required. The chin bone is cut using an incision inside the mouth and the chin is moved forward or lengthened vertically in patients with small chins. The advanced chin is held in place with a small metal plate and tiny screws. The surgery does not move teeth or affect occlusion. This operation takes approximately one hour to complete.
What results can I expect?
The results of your procedure are visible almost immediately. Initial swelling will subside over the first week with the use of cold compresses, and continue to subside for the following two to four weeks. After chin surgery, your chin will be swollen, firm and possibly bruised. Using cold compresses in the first 48 hours will significantly lessen the swelling, as will keeping your upper body elevated when resting.
What is involved in recovery?
Recovery from chin surgery involves some swelling, bruising and numbness for several weeks following surgery. You’ll have incisions in your mouth, increasing the risk for infection from the bacteria that normally reside there, so be especially attentive to caring for your mouth (oral hygiene) according to your surgeon’s instructions. During the recovery period, you’ll need to eat only soft foods and protect your face from bumps and other injuries.
Is chin surgery procedure safe?
All surgical procedures carry some risk.
Possible complications from chin surgery include:
• Bleeding (hematoma)
• Infection
• Poor healing of incisions
• Anesthesia risks
• Change in skin sensation due to nerve injury
• Swelling
• Bruising
• Skin contour irregularities
• Skin discoloration and swelling
• Pain
• Skin sensitivity
• Blood clots
• Possibility of revisional surgery
